|
In this edition of "What the Hell? - Cancer" I will going through how cancers are diagnosed. This will hopefully give you an idea about what the different stages of cancer are and how each cancer is graded differently.
NOTE: All my examples will be using breast cancer because it is the cancer type I study and am most familiar with. Before I begin I want to just clear up the differences between primary tumours, secondary tumours and primary secondary tumours.
Cancer diagnosis is a tricky business. If you read my awareness posts you will see the signs and symptoms of a lot of different cancers. You may have noticed that a lot of the signs and symptoms are generic for example bloating, intestinal discomfort, a prolonged cough etc.
Detection
Tumours need to be detected before you can take a biopsy etc. These are the main ways tumours are detected (but not the only ways). Apologies for the explanations. While I learnt all this in my masters (woo nuclear physics) I am no physicist...
Pathology
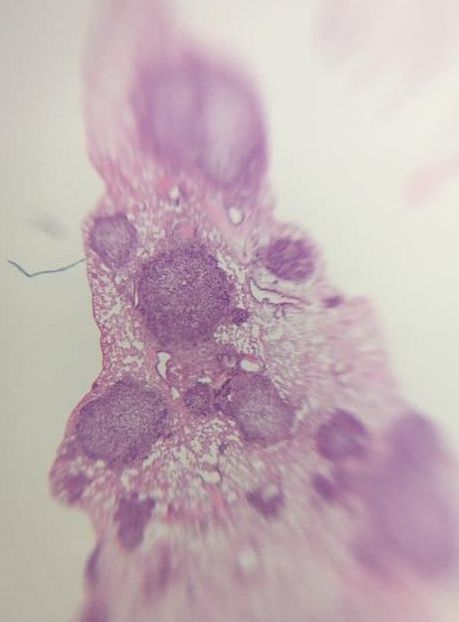
Part of what pathologists are looking for when they stain biopsies is structural changes to cells. Cells "adapt" to their environment or from internal cues by changing their structure. There are a number of cellular adaptions which happen normally but can also be due to disease etc.
The next three are characteristic of pre-cancer cells (i.e. structural changes that can lead to cancer):
Change of shape and structure and the number of darkly stained cells allow pathologists to grade tissue samples. Histopathology is based very much on the person and takes years and years to generate enough knowledge to be able to look down a microscope at a purple stained piece of tissue and say "that is a squamous cell carcinoma" (type of skin cancer - don't look up images). There is a lot more to the work of a pathologist but I don't have the knowledge to delve deeper. Staging and Grading
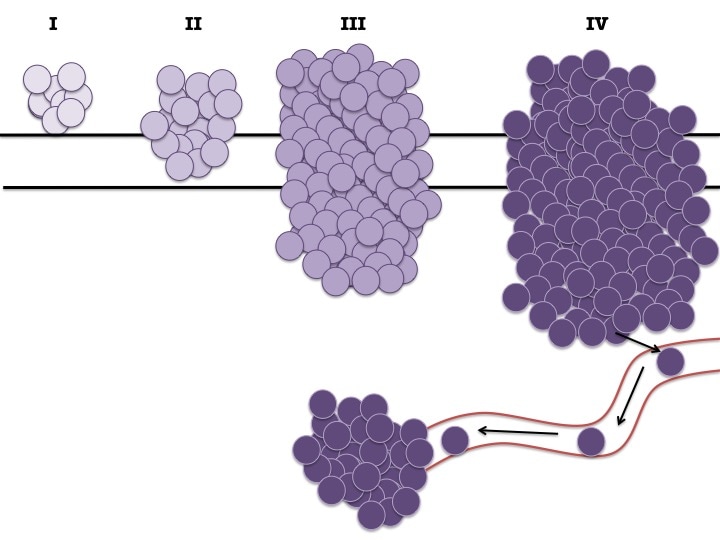
So what do I mean by stage? Well the stage of the cancer tells you (in general terms) how big the tumour is, if it has invaded locally or systemically and what treatment you should use.
Clinicians expand on this and use a system called TNM. This is "Tumour", "Node", "Metastasis".
As I said before each cancer type has slightly different staging criteria. This is due to the type of organ it is in (some organs are smaller than others so a "small" tumour in a large organ is actually quite a big tumour in a smaller organ). The staging also has to take into account where the tumour invades locally and systemically and if lymph nodes are involved.
In breast cancer:
Other cancers like Colorectal Cancer use additional staging techniques for example Duke's Staging which is very like the numbered system but is marked by grade A-D. Location/Origin
But the above is not the only way to identify the type of cancer! Oh no, like all aspects of cancer biology there is always more.
While the stage/grade will help you with treatment options there are other factors such as location that tell you about the cancer. For example in breast cancer: Epithelial Tumours:
Other:
Mutations and Chromosomal Changes
And as always we come back to DNA. There are mutations that are common in pretty much every cancer type (e.g. p53) but other mutations are specific to certain cancers of families of cancers. For example BRCA mutations are associated with both breast and ovarian cancers.
In breast cancer the common mutations used to define cancer types are:
In breast cancer if you have suspected Her2+ cancer a number of tests are done such as Immunohistochemistry (IHC) which detects Her2 receptor levels on the surface of the breast cancer cell and Fluorescence In Situ Hybridisation (FISH) which detects the number of copies of the HER2 gene there are. There are genetic screening tests used in the clinic for some cancers. In breast cancer there is OncotypeDx which detects 21 genes commonly mutated in breast cancer. This gives you a score. OncotypeDx also has systems for prostate and colon cancer. Changes to the chromosomes themselves are also common, usually in haematological malignancies.
In chronic myelogenous leukaemia (CML), there is a translocation called BCR-ABL where part of the chromosome where the ABL gene is located (Chr.9) breaks off and switches with the part of the chromosome where BCR is located (Chr.22). This brings BCR and ABL together creating a powerful oncogene.
And you combine them all. You take your image of the tumour(s) with all of the measurements and origin of the primary tumour, you get the pathologists report from the biopsy about the type of cancer it's believed to be, how fast it's growing, what proteins it may be expressing on the cell surface and how aggressive it is and lastly genetic testing to determine the mutations. This gives you a picture which allows you to provide the best treatment plan for that patient.
So a patient could have a T2N1M0 ER+ invasive lobular breast carcinoma, meaning they have a breast cancer which originated from the epithelial cells in the lobes of the breast, the cells show structural changes and it is between 2cm and 5cm across, there 1-2 lymph nodes with infiltrating breast cells, there is no metastasis and the tumour is oestrogen receptor positive. The treatment path for this patient may be surgery to remove the tumour and lymph nodes involved or a full mastectomy. Depending on the surgery, the patient may receive chemotherapy and will more than likely be given tamoxifen (anti-oestrogen receptor drug) for 5-10 years. It's difficult to describe every type of cancer's staging systems because as I said it really is dependent on the type of tumour.
And that is the basics of it. As always if you have questions please don't hesitate to ask. This isn't all of the information and if you or someone you know is affected by cancer they should ask their attending physician to explain their diagnosis to them (cancer is so nuanced).
Hopefully in the next month or so I will put up our penultimate "What the Hell? - Cancer" blog post on Cancer Treatment! For more information check out CRUK's website https://www.cancerresearchuk.org/
0 Comments
|
AuthorMy name is Caitriona and I am a PhD student at Imperial College London, UK. Categories
All
|